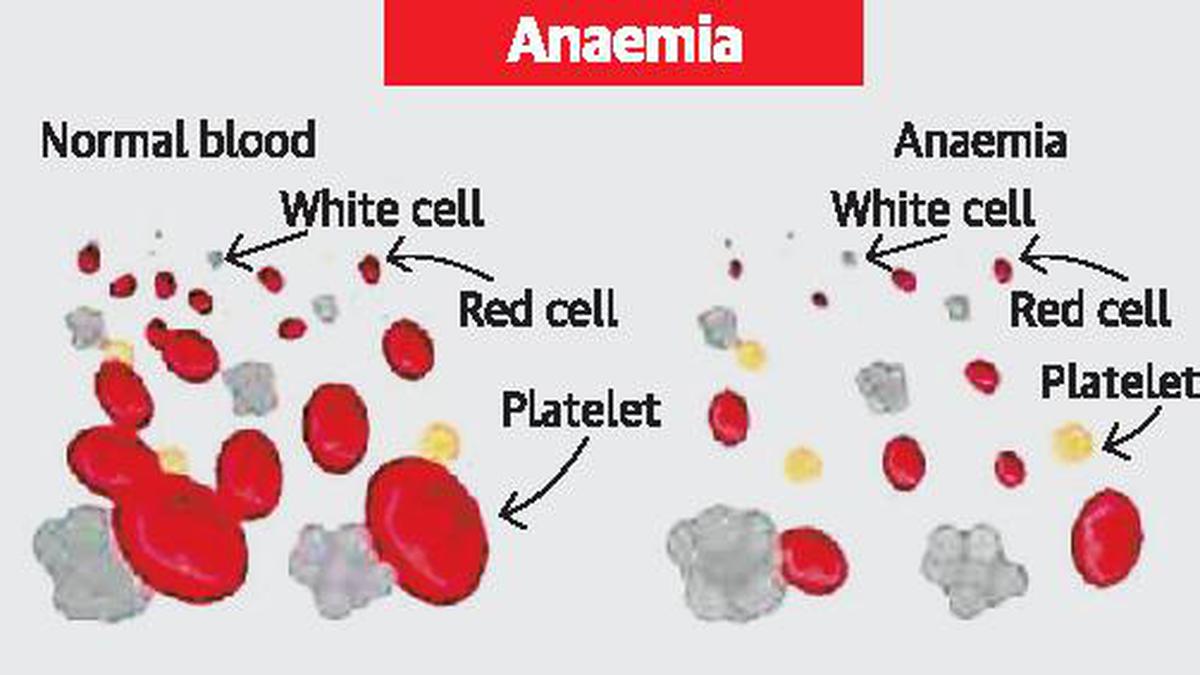
In my nearly four decades of practice, one recurring reality has stood out — far too many women begin pregnancy already struggling with undiagnosed anaemia. Maternal health in India is often viewed through the lens of pregnancy and childbirth, but its foundation is laid much earlier — long before conception. A woman’s health at the time of conception shapes not only her pregnancy but also the well-being of her child. Yet, for more than 57% of women in their reproductive age in India, this foundation is weakened by undiagnosed and untreated anaemia. These women experience persistent fatigue, dizziness, and weakness, yet these symptoms are more than often dismissed as routine. By the time they conceive, their haemoglobin levels are already dangerously low, increasing the risk of preterm birth, low birth weight, and life-threatening maternal complications such as pre-eclampsia and post-partum hemorrhage, all of which contribute to maternal and perinatal morbidity and mortality.
While efforts to improve maternal health have helped bring down the Maternal Mortality Ratio to 93 per 1,00,000 live births in India, sustaining and accelerating this progress requires a shift in approach. Achieving further reductions, and aligning with the Sustainable Development Goals, means going beyond interventions during pregnancy to include proactive measures much earlier. To truly transform anaemia prevention and management, we must reframe the approach to emphasise preconception health. The question should not only be, “Are you ready for motherhood?” but also, “Is your body ready for pregnancy?”
A comprehensive approach
For decades, oral Iron-Folic Acid (IFA) supplementation has been the primary strategy for preventing and managing anaemia. While beneficial, oral IFA has limitations — many women struggle with nausea, loose motions, constipation, and poor absorption, leading to low adherence. Moreover, for women with long-standing anaemia, the short window of pregnancy is often insufficient to restore their iron levels through oral supplements alone. As a consequence, there is reduced transfer of iron to the infant as well, causing anaemia.
A more comprehensive approach is needed to effectively manage moderate to severe anaemia and prevent its progression during and after pregnancy. Here, Intravenous Ferric Carboxymaltose (IV FCM) presents a safer and more effective alternative. Unlike oral iron, IV FCM delivers iron directly into the bloodstream, rapidly restoring haemoglobin levels and iron stores. This is not affected by Hepcidin levels unlike oral iron.
While Iron Deficiency Anemia (IDA) is the most common cause of anaemia, it is not the only one. Vitamin B12 deficiency is often overlooked, despite its crucial role in red blood cell formation and neurological function. A study found that nearly 49% of women of reproductive age suffer from Vitamin B12 deficiency with an impact on anaemia and birth defects. Without adequate Vitamin B12, iron supplementation alone cannot fully address anaemia. In addition, undiagnosed thyroid disorders, such as hypothyroidism or hyperthyroidism, can mask or exacerbate anaemia and negatively impact foetal development. Similarly, many Indian women remain unaware of their gestational diabetes status until later stages of pregnancy. Screening for thyroid function, blood glucose levels, and Vitamin B12 deficiency before conception can significantly improve pregnancy outcomes and overall maternal health. It is better to combine injectable Vitamin B12 and Folate along with IV Iron to prevent refractory anaemia.
Shifting to an approach that is focused on preconception health requires community involvement. As families influence health decisions, they should encourage preconception health check-ups. Accredited Social Health Activists and Anganwadi workers should incorporate preconception health education into existing maternal and child health programmes. Their proximity to communities uniquely positions them to highlight the importance of preconception screening, ensuring women recognise that these check-ups are as critical as antenatal visits in preventing life-threatening complications.
A societal imperative
Improving maternal health is not merely a medical responsibility; it is a societal imperative. Families, healthcare systems, policymakers, and communities must work collaboratively, proactively, and with sustained commitment. Failing to address anaemia and other deficiencies before conception does a disservice not only to women, but also to future generations whose potential begins before birth.
By normalising preconception check-ups, expanding the use of newer interventions such as IV FCM, and refining existing oral IFA strategies (especially administration patterns — daily versus alternate or twice-weekly), we can provide every mother in India with the opportunity for a safe, healthy, and dignified pregnancy.
The time for action is now. No woman should enter pregnancy anaemic. No woman should be anaemic during pregnancy due to preventable deficiencies. No woman should leave childbirth weaker than she entered it. Making preconception care as routine as antenatal care is not optional — it is essential, urgent, and transformative. If we want our next generation to be healthier and smarter (as iron influences foetal and infant brain development), mothers must be healthy at the start of pregnancy.
Mrutyunjaya Bellad, Professor, Department of Gynaecology and Obstetrics, Jawaharlal Nehru Medical College, Belgaum, Karnataka
Published – May 27, 2025 02:27 am IST